Physician Associates
October 2024
The RCGP has published guidance on induction and preceptorship, supervision and scope of practice of Physician Associates (PAs) working in general practice. This follows a member consultation conducted by the College in April and May 2024, the results of which have been used to inform this guidance. The final guidance was approved by RCGP UK Council in September 2024.
In September 2024, Council also voted to oppose a role for PAs in general practice. However, in recognition that responsibility ultimately rests with employers and that there are already around 2,000 PAs working in general practice, this guidance is intended as a practical resource for GPs and practices where PAs are employed.
September 2024
The RCGP's governing UK Council has today voted to oppose a role for Physician Associates working in general practice.
The outcome of the vote was 61% of Council Members agreeing to oppose the role of PAs working in general practice; 31% disagreeing; and 8% abstaining.
However, recognising that there are already around 2,000 PAs working in general practice, RCGP Council did approve three sets of guidance to support GP practices already employing PAs. The guidance will cover the induction and preceptorship, supervision, and scope of practice of PAs currently working in general practice. This guidance has been informed by and reflects the results of the member consultation on the use of PAs in general practice conducted by the College in April and May this year, and the ‘red lines’ affirmed by UK Council in March 2024.
Council opposed inclusion of a paragraph in the draft scope of practice guidance that where existing PAs in general practice may currently be practising beyond the scope described in our guidance, it is the responsibility of their GP Clinical Supervisor and/or their employer, to determine that they are doing so safely. This paragraph will be removed to ensure it is clear that PAs must always work within the scope of practice the RCGP will set out.
The College will now undertake further work on these documents, taking on board comments made by Council Members, and publish them as soon as possible.
Given that there are PAs currently working in general practice, the principles set out in the College’s ‘red lines’, agreed in 2017 and strengthened at its Council meeting in March 2024, still stand.
It also remains the College’s position that the regulation of PAs must proceed as soon as possible. It is the RCGP's position that a regulatory body other than the GMC would be more appropriate to take forward this crucial work - but recognising that GMC regulation is well advanced, and now in legislation, the College will continue to work with the GMC to ensure there is clarity over the differences between doctors and PAs.
June 2024
The RCGP is today (20 June 2024) publishing the results of our member survey on the role of Physician Associates (PAs) in general practice. The survey takes forward the decision of our UK Council to conduct a member consultation and to use this to inform the production of College guidance on this subject.
We are grateful to all our members who have given their time and expertise to complete the survey and to feed back on their views and experience regarding the deployment of PAs in general practice.
A comprehensive presentation, setting out in detail the quantitative results from the survey, together with a thematic analysis of some of the free text responses, has been produced by Research by Design. Read the full PA survey results report (PDF file, 1.1 MB).
You can also read data tables of the quantitative survey results (XLSX file, 1.6 MB).
The survey was open to all RCGP members training as a GP in the UK and all those who are currently, or have previously, practised as a GP in the UK. A direct email was sent to all members on our database who were listed as either based in the UK, or who had trained in the UK but were currently based abroad. It received 5112 responses, equating to approximately a 10% response rate, and was designed to protect the anonymity of respondents. The survey was conducted and analysed by the independent research company, Research by Design. The demography of the survey was representative of the RCGP membership in terms of GP Registrar/Associate in Training : Member ratio and male : female ratio, and therefore the responses have not been weighted.
There were some differences between the responses from GP Partners and those from other roles regarding current and previous experiences with PAs (shown in section 2 of the report) and the picture varied slightly between different questions. However, in general there was relatively little variation in the responses given by respondents at different career stages, and between those with and without experience of working with PAs in general practice.
A comprehensive presentation, setting out in detail the quantitative results from the survey, together with a thematic analysis of some of the free text responses, has been produced by Research by Design. Read the full PA survey results report (PDF file, 1.1 MB).
You can also read data tables of the quantitative survey results (XLSX file, 1.6 MB).
We will be working with Research by Design to conduct further analysis of the free text responses as part of our next steps and using the insights from this to inform the development of our work in this area.
The responses to the survey highlight the wide variability in the way PAs are currently deployed, inducted and supervised in general practice, with clear findings that in many places these processes are not as robust as they should be. Across a range of areas, there were significant differences between the ways in which respondents said PAs are currently working compared to the ways in which respondents said they should be working.
Some of the key concerning results include:
- 81% of all respondents said that they considered negative effects on patient safety to be one of the challenges of the use of PAs in general practice.
- 50% of all respondents reported being aware of specific examples of patient safety being compromised by the work of PAs, with common themes including misdiagnosis and diagnostic errors by PAs, inappropriate prescribing and management, and lack of communication to patients and GPs.
- 60% of all respondents with experience of working with PAs said that PAs in their practice act as the first point of contact for potentially serious conditions (falling to 48% of GP Partner respondents with experience of working with PAs).
- Furthermore, the survey results suggest that standards of induction and supervision are often inadequate:
- Only 25% of all respondents with experience of working with PAs said that all PAs had an annual appraisal (rising to 59% of GP Partner respondents with experience of working with PAs).
- 25% of all respondents with experience of working with PAs said that no time was scheduled for regular supervision of PAs, meaning PAs could only speak to their GP supervisor in gaps between appointments (rising to 31% of GP Partner respondents with experience of working with PAs).
- Even discounting the lack of regulation and the lack of adequate resources for training, induction and supervision, 24% of respondents said that they are aware of cases where the College’s 'red lines' (below) are being breached.
We recognise that the picture emerging from these results is disturbing, and will be of concern to many, including patients, GPs and PAs themselves. The RCGP has stated that, within the right framework and parameters, PAs have the potential to make a useful contribution to general practice, and we are mindful that there are also reports from the survey of where the role has worked well. However, it is also clear that in a significant number of reported cases, there is not a sufficiently robust framework for supervision and scope of role in place in practices. Our respondents fed back that more work was needed to provide greater clarity on what activities PAs should and should not undertake within general practice, and the standards of induction, training and supervision necessary to allow them to be deployed safely with patients. In addition, urgent action from government and NHS leaders will be required to support general practice to deliver on these standards, including the implementation of a robust system of professional regulation and significantly increased resourcing for PA supervision.
After consideration of the survey results, and mindful of the RCGP’s Charitable Purpose to ‘encourage, foster and maintain the highest possible standards in general medical practice’, we are recommending to our members that they review their recruitment plans and halt the recruitment and deployment of additional PAs into general practice across the UK until PAs are regulated and practices are in a position to implement the RCGP's forthcoming guidance.
This is a difficult step to take, but we feel that with the evidence we have collected and considered from the consultation, to continue to bring additional PAs into general practice at the present time would not be in the interests of patients, the PAs themselves, or the GPs who are clinically responsible for them.
We are also very aware of those Physician Associates who are already employed within general practice settings at a time which is unsettling, and of general practice's responsibilities towards them as employers and supervisors, and to the patients they care for. The College is working to produce guidance for our members on the role and use of PAs in general practice settings, including their scope of practice, induction and supervision arrangements, which we intend to bring to our September meeting of UK Council for approval. In the meantime, we recommend that all practices currently utilising PAs should review their induction, supervision and triage processes, as well as the type of work that PAs are undertaking, in order to assure themselves that the College’s existing red lines are not being breached:
- PAs working in general practice must always work under the supervision of qualified GPs.
- PAs must be considered additional members of the team, rather than substitutes for GPs.
- PAs do not replace GPs or mitigate the need to urgently address the shortage of GPs.
- PAs must be regulated as soon as possible.
- Public awareness and understanding of the PA role must be improved.
- Training, induction and supervision of PAs within general practice must be properly designed and resourced.
- At a time of significant GP workforce challenges, funding allocations, resources and learning opportunities within general practice must be prioritised for the training and retention of GPs.
- The significant responsibility and skills required for supervision must be recognised and resourced, with GPs able to choose whether or not they are willing to undertake supervision of PAs. PAs should not be employed unless sufficient supervision can be provided.
In addition, and based on the survey results, we recommend that GPs and practices take steps to ensure that:
- Appropriate time for supervision is be included within GPs' and PAs’ daily timetables.
- Processes of triage, induction, and supervision are reviewed to ensure they are robust and safe for patients, and all PAs have documented annual appraisals.
- PAs do not see patients who have not been triaged by a GP and only undertake work delegated to them by, and agreed with, their GP supervisor. This work must be in line with the agreed scope of role for that PA in the practice.
- Transparent and accurate methods of introduction of all members of the MDT seeing patients are visible to patients, including on the practice website, on consulting room doors, on name badges and when appointments are booked.
- Patients who have already consulted a PA for a problem, and who re-present again with the same problem which has not been diagnosed and resolved, should not re-consult a PA, but should see a GP.
We recognise that that there may be exceptional circumstances in which practices choose to go ahead with recruitment of PA roles, but they need to be aware of these recommendations and be absolutely sure that the arrangements they make are robust and safe for patients. In these circumstances it is essential that employers take specific measures to assure themselves of the skills and experience of the individual in question, and that a clearly defined scope of practice is agreed in advance of employment starting.
- Governments across the UK must urgently take action to grow the GP workforce and ensure that, as per our red lines, PAs are not used as substitutes for GPs or to mitigate the need to urgently address the shortage of GPs.
- Governments across the UK should commission an urgent review of the ways in which PAs work in the NHS.
- Governments across the UK should ensure appropriate resources are provided to support multidisciplinary team (MDT) working within general practice. This must cover appropriate induction – including mandatory primary care preceptorships for PAs, supervision, MDT teamworking and integrated communication within the practice team, with the wider primary healthcare team, and with social care teams.
- Regulation of PAs must proceed as soon as possible. It is the RCGP's position that a regulatory body other than the GMC would be more appropriate to take forward this crucial work. However, given GMC regulation is well advanced, and now in legislation, the RCGP will continue to work with the GMC to ensure there is clarity over the differences between doctors and PAs.
Using insight gathered from the survey results, as well as further external stakeholder and member engagement, the RCGP will develop UK wide guidance on scope of practice, induction and supervision of PAs in general practice. This will be brought to the meeting of RCGP UK Council in September 2024 for approval prior to publication.
May 2024
Thank you to the over 5,000 members who responded to our member survey on the role of PAs in general practice. This survey is now closed and we are working carefully on the analysis to ensure that all of the responses and important issues raised can be properly considered. We will publish the results in June, and following this we will be working to address the issues raised and develop guidance for members.
April 2024
Following the discussion at UK Council in March, the RCGP is proceeding with a member consultation on the role of PAs in general practice. A survey of all current RCGP members who are training as a GP in the UK and those who have practised as a GP in the UK, is running from 22 April to 10 May 2024. The survey aims to gather the views and experiences of RCGP members. It is designed to collect as much information as possible to help inform the internal Task and Finish Group which will be developing subsequent guidance, and this will be taken to RCGP Council for approval prior to publication. Research by Design is an independent market research company which has been commissioned by the RCGP to undertake this survey research on its behalf.
Our survey and wider consultation process seeks to understand how PAs currently work in general practice, including what types of work they undertake and what supervision is in place. It also considers the potential benefits, and challenges and concerns related to the PA role in general practice. Building on this, it seeks to establish views on what framework and parameters should be in place to ensure PAs can work safely and effectively in general practice, and what guidance is needed from RCGP to this end.
If you are an RCGP member and you have not received an email with the survey link from Research by Design by Tuesday 23 April 2024 and believe that you should have, please contact us at policy@rcgp.org.uk.
March 2024
Following discussion at its UK governing Council meeting on 8 March 2024, the Royal College of General Practitioners has strengthened and updated its position on the role and regulation of Physician Associates (PAs) working in general practice.
The Council confirmed the College’s existing ‘red lines’ on PAs, and voted to add two more, explicitly stating that the training and retention of GPs must be prioritised and that the responsibilities and skills required by GPs to supervise PAs must be recognised and resourced.
The RCGP’s updated position now stipulates:
- PAs working in general practice must always work under the supervision of qualified GPs.
- PAs must be considered additional members of the team, rather than substitutes for GPs.
- PAs do not replace GPs or mitigate the need to urgently address the shortage of GPs.
- PAs must be regulated as soon as possible.
- Public awareness and understanding of the PA role must be improved.
- Training, induction and supervision of PAs within general practice must be properly designed and resourced.
- At a time of significant GP workforce challenges, funding allocations, resources and learning opportunities within general practice must be prioritised for the training and retention of GPs.
- The significant responsibility and skills required for supervision must be recognised and resourced, with GPs able to choose whether or not they are willing to undertake supervision of PAs. PAs should not be employed unless sufficient supervision can be provided.
Whilst continuing to recognise that regulation of PAs is vital and must happen as soon as possible, Council members raised significant concerns that PA regulation by the General Medical Council could increase confusion amongst patients about the differences between doctors and PAs. It was therefore passed by Council vote that the RCGP should change its stance on this issue and that another regulatory body would be more appropriate to take this crucial work forward to regulate PAs. Regardless of the regulatory body, as previously stated, it is also important that any costs of the regulation of PAs must not be transferred to doctors. Given legislation was passed through the House of Lords last week, the RCGP will need to enter into discussion with the GMC and other key stakeholders to look at how these concerns can be addressed.
Council also agreed that the RCGP should consult with members on the role of PAs in general practice settings, including their scope of practice and supervision arrangements. This consultation will commence in the coming weeks and will inform the development of College guidance.
February 2024
We have briefed Lords ahead of a debate on regulation of Physician Associates and reiterated our red lines in relation to the role within general practice:
- PAs working in general practice must always work under the supervision of qualified GPs.
- PAs must be considered additional members of the team, rather than substitutes for GPs.
- PAs do not replace GPs or mitigate the need to urgently address the shortage of GPs.
- PAs must be regulated as soon as possible.
- Public awareness and understanding of the PA role must be improved.
- Training, induction and supervision of PAs within general practice must be properly designed and resourced.
We similarly briefed MPs ahead of a debate in the House in Commons in January.
The role of PAs in general practice will be discussed further at our Council meeting in March.
October 2023
The RCGP Council agreed the position below on Physician Associates in 2017. In the intervening period, the College has continued to monitor developments around the role and to work to ensure appropriate implementation and integration.
The RCGP position is that Physician Associates have an enabling role to play for general practice. They are members of the multidisciplinary team, trained in the medical model, and can help broaden capacity and skill mix within the practice team, assisting GPs and their teams to provide high-quality, integrated care.
We are very clear that Physician Associates must always work under the supervision of GPs and must be considered complementary/additional members of the team, rather than a substitute to GPs. They must not and do not replace GPs and do not mitigate the need to urgently address the shortage of GPs, which is even more acute now than it was in 2017.
It is disappointing that many of the actions we called for in 2017 to ensure Physician Associates in general practice could be safely and effectively integrated into the multidisciplinary team have not yet been delivered. It is clear that much greater guidance, support and regulation are urgently required.
Regulation
It is positive that the GMC is proceeding with professional regulation of Physician Associates in all settings. This is very important and needs to be implemented as quickly as possible. We understand this is not currently expected until at least the second half of 2024, which will mean challenging implications in the interim. This must be urgently prioritised by the GMC and the Government.
Public awareness
Important concerns have been raised about public awareness of the different roles within the MDT, and specifically of the role of Physician Associates. We welcome the Faculty of Physician Associates' 2023 titles and introduction guidance which gives helpful clarity on the role of Physician Associates and guidance on how to make introductions when consulting with patients. The RCGP has consistently called for greater public education around the different MDT roles and are continuing to work with NHS England on this.
Training, induction and supervision
It is important that Physician Associates spend a significant proportion of their training within general practice, just as it is important for trainee doctors and all members of the MDT. As highlighted in our GP infrastructure report, there is a severe lack of training capacity, both in terms of lack of space and a shortage of educators and supervisors. It is therefore important that resources are provided to increase MDT training placements in general practice for Physician Associates, and others, bearing in mind that GPs also supervise and train GP trainees and medical students. Once Physician Associates are trained they must always work under the supervision of a GP, and therefore the resource implications of supervision also need to be properly accounted for and funded.
October 2017
This paper sets out the RCGP position on the role of Physician Associates in general practice. It frames the current situation and explores the key challenges that need to be resolved to support Physician Associates to work most effectively and safely in general practice.
The RCGP is committed to working with governments across the UK, the Faculty of Physician Associates and our membership. We aim to ensure that Physician Associates in general practice are safely and effectively integrated into the multidisciplinary team. Physician Associates are new members of the clinical team. Complementary to GPs rather than a substitute, who assist GPs and their teams to provide high-quality, integrated patient care.
Physician Associates can fulfil an enabling role for general practice. They are taking on specific workload areas, helping to free GPs to focus on the more complex patient cases and other staff, such as nurses, to focus on their competency areas. They can also free up GPs to carry out other important activities, such as training, Continuing Professional Development (CPD) and research.
One of the key aims of integrating Physician Associates is to ensure that GPs can continue to lead multi-disciplinary teams. These teams can adapt to the evolving healthcare needs of patients in response to a growing and ageing population. This does not mitigate the need to address the shortage of GPs supervising their work urgently. It does not reduce the need for other practice staff. Instead, Physician Associates can help broaden the GP role's capacity and skill mix within the practice team to enhance patient care.
The next steps for integrating Physician Associates into general practice should include:
- Commitments relating to Physician Associates in the GP Forward View need to be met. These sit alongside commitments to increase the number of GPs
- Professional regulation needs to be established as a matter of urgency
- Once regulated, consideration needs to be given to enabling Physician Associates to acquire appropriate prescribing rights
- The level of exposure to general practice during Physician Associate courses needs to be evaluated and potentially extended
- Resources for training placements in general practice must be increased; accordingly, the training of GPs and other staff must not be affected
- Clearer guidance and support needs to be produced on effective supervision of Physician Associates, e.g., in out of hours settings
- Funding should be provided to practices to support Physician Associate’s transition into employment, e.g., for preceptorships
- Further research is needed on the cost, impact and geographical distribution of Physician Associates
- Measures should be taken to raise public awareness and understanding of the Physician Associate role in general practice
Please note - a case study previously included as part of this statement has been removed at the request of the individual. This well respected and experienced health professional acted in good faith by generously allowing the case study to be used when we originally published the page in 2017. However, it has been brought to our attention that, due to an error by the College, editorial changes were later made to it, without the subject’s knowledge and which made the case study factually incorrect. The College takes full responsibility, and we apologise unreservedly. At no point has the individual been at fault.
- Physician Associates are healthcare professionals with a generalist medical education who work under the supervision of doctors providing medical care to patients. They are dependent practitioners who work with a doctor as a named supervisor, but are able to work with some autonomy with appropriate support.
- The Department of Health defines a Physician Associate as:
A new healthcare professional who, while not a doctor, works to the medical model, with the attitudes, skills and knowledge base to deliver holistic care and treatment within the general medical and/or general practice team under defined levels of supervision (Department of Health, 2012). - Physician Associates are still relatively new to the NHS. New UK Physician Associate courses have only produced graduates since 2007 (Drennan, et al., 2015). The Faculty of Physician Associates believes there are up to 450 Physician Associates in the UK working throughout the NHS. In a recent survey conducted on behalf of the UK and Ireland University Board for Physician Associate Education (UKIUBPAE) and Health Education England (HEE), which had a 100% response rate from universities that conduct Physician Associate courses, there were 1,210 Physician Associate students in the UK (Parle. J, 2016). As of 4th August 2017 there were 366 registered as Physician Associates on the Managed Voluntary Register with the Faculty of Physician Associates (Faculty of Physician Associates, 2017b).
- The first Physician Associates were trained in the USA where they are known as Physician Assistants. Here, Physician Associates are a well-established and regulated profession. Around 100,000 work across the USA, of whom around 30% work in primary care (Anadalo, 2016). There are approximately 40 Physician Associates working in the UK who trained in the USA (Parle. J, 2016).
- Governments across the UK are at different stages of developing and implementing the role of the Physician Associate in general practice:
- In England, the General Practice Forward View (GPFV) commits to investment by HEE in the training of 1,000 Physician Associates to support general practice by 2020
- In Scotland, the Government has not taken a stance on Physician Associates in general practice although it has been very supportive of enhancing the multidisciplinary team
- In Wales, the Government has established a Physician Associate Workforce Development Group. In 2016, the government began funding the first year of the Physician Associate course in Swansea and Wrexham
- In Northern Ireland, the Department of Health has been supportive of the Physician Associate concept
Geographical distribution
- While anecdotal feedback from GPs working with Physician Associates has generally been positive, discussions have highlighted some concerns among doctors about the role of Physician Associates, including:
- Lack of professional regulation
- Lack of clarity among doctors, patients and the public about Physician Associates and their roles
- Concerns about the impact of PAs on doctors’ training
- Lack of clarity about supervision
- Suitability of Physician Associates to different care settings
- Physician Associates as a quick and cheap substitute for fully qualified doctors (British Medical Association, 2017)
- Understanding patient views of Physician Associates is critical for this discussion. The views of the RCGP’s Patient Groups across the UK were sought via a survey and have been incorporated into this paper. Members of the RCGP’s Patient and Carers Partnership Group were also consulted in the development of the paper.
- In the UK, Physician Associates are currently predominantly based in England. The table below summarises the census results by the Faculty of Physician Associates (Ritsema T. S., 2016). It should be noted that the census response rate was 58.2%, and there are likely to have been developments since the census last year; for example, anecdotal evidence indicates that a few Physician Associates are starting to gain employment in Wales.
| Percentage of Physician Associates employed in each nation of the UK | |
| England | 87% |
| Scotland | 12.5% |
| Wales | 0% |
| Northern Ireland | 0.5% |
Physician Associates in general practice
- Data published on 22nd August 2017 by NHS Digital indicates that there were 48 FTE (58 headcount) Physician Associates working specifically in general practice as of March 2017 (NHS Digital, 2017).
The role of a Physician Associate in general practice
- Physician Associates are in patient-facing roles and in general practice they see patients in their own appointments. As Physician Associates are dependent practitioners, they are supervised by a GP, and they cannot currently prescribe. The scope of practice for any particular Physician Associate will therefore develop over time at the discretion of their named supervising GP, who has overall responsibility for the Physician Associate. As with other roles, the named supervising GP does not have to be present at all times that the Physician Associate is working; their day-to-day work can be overseen by any GP that is present at the time. This can be structured in different ways, but anecdotal examples include lunchtime meetings with a GP and sometimes the wider team, ad hoc advice where appropriate for urgent complex referrals, and meetings at structured points in the day for GPs to sign prescription requests.
- The Faculty of Physician Associates states that:
In a GP surgery, Physician Associates see patients of all ages for acute and chronic medical care. Physician Associates can refer patients to consultants, the Emergency Assessment Unit (EAU) or to A&E when clinically appropriate. Other duties include home visits, prescription reauthorisation, review of incoming post and laboratory results. Physician Associates are an additional health care team member to help the practice reach Quality Outcome Framework targets (Faculty of Physician Associates). - Perhaps unsurprisingly, given the relatively small numbers working in UK general practice, there currently needs to be more research on the safety and effectiveness of Physician Associates in general practice. One study by Drennan et al. (2015) compared aspects of Physician Associate consultations with those of GPs. The study found similar processes and outcomes of Physician Associate and GP consultations for same-day minor illness patients. In contrast, the cost of a Physician Associate consultation was lower. Anecdotal evidence from GPs working with Physician Associates suggests that Physician Associates can contribute to reducing GP workload and freeing up GP time to care for more complex patients.
- Physician Associates have a different expertise in medical generalism than GPs. They can only have supportive and complementary roles to GPs. They cannot act as a substitute for GPs, with their unique skill sets in areas such as diagnosing undifferentiated symptoms, managing uncertainty and treating multiple conditions. GPs remain the only professionals who can take a holistic medical diagnosis of the whole person, combining physical, psychological and social aspects of care for all patients, including those with the most complex needs.
- A study in Scotland looked at an example of a scope of practice for a Physician Associate working in general practice. It included the following tasks:
- Elicit a comprehensive history
- Elicit a problem-oriented history
- Perform a complete and directed physical examination
- Formulate a differential diagnosis
- Formulate a patient-focused management plan of care
- Order appropriate tests and interpret test results
- Prepare prescriptions for signature
- Educate and counsel patients and families
- Arrange for follow-up care and/or referrals to specialists
- Perform injections, aspirations, basic phlebotomy, dipstick urinalysis, collection and preparation of cultures, fluorescin exam, minor surgery, diagnostic tests, take vital signs
- House calls for nursing and homebound patients (Farmer, Currie, West, Hyman, & Arnott, 2009)
Multidisciplinary team working
- Physician Associates are trained to work as part of a multidisciplinary team in general practice. Their exact role will depend on the make-up of the wider team, which can vary widely. In addition to being supervised by and working with GPs, Physician Associates may work with:
- General practice nurses including Advanced Nurse Practitioners
- Healthcare assistants
- Clinical pharmacists
- Paramedics
- Mental health therapists
- Physiotherapists
- Practice managers
- Reception and clerical staff
- A study in Scotland found that team members working with Physician Associates found they brought additional complementary skills and attitudes to teams but should not be regarded as a potential direct substitute for a nurse or a doctor (Farmer, Currie, West, Hyman, & Arnott, 2009).
Training
- The first Competence and Curriculum Framework for the ‘Physician Assistant’ (later changed to Physician Associate), was developed in 2006 by the Department of Health in partnership with RCGP and the Royal College of Physicians (RCP). The initial framework drew from the American model which had been established for over 40 years (Department of Health, 2006). This helped to form the basis for the Department of Health’s revised curriculum framework for Physician Associates in 2012.
- The current curriculum framework specifies that Physician Associates will complete a Masters level 1 academic programme of no less than 90 weeks leading to a Postgraduate Diploma in Physician Associate Studies. It also recommends that newly qualified Physician Associates undergo a period of preceptorship, during which they receive additional training in relation to the clinical field in which they are working as well as consolidating their common core learning and providing a clinical service (Department of Health, 2012). Some regions are developing general rotations which are somewhat similar to foundation years, e.g. 16-month periods with three 4 month placements in hospitals and one in general practice. Other regions are focusing specifically on ‘first contact’ services. In these areas Trust A&E departments are working with general practice provider organisations to provide a period of experience in both areas. Preceptorships such as these are seen as potential ways of attracting qualified Physician Associates to work in a particular region.
- In England, there were 28 Physician Associate courses as of August 2017 (across 26 institutions: see Appendix 1 for the full list). In Scotland, there is a Physician Associate course at the University of Aberdeen. Physician Associate courses have recently started in Wales at Bangor and Swansea Universities, and in Northern Ireland at Ulster University. Physician Associate students usually have an undergraduate qualification in a life science field, although some Physician Associates have experience as nurses, healthcare assistants or paramedics (Faculty of Physician Associates).
- Physician Associates have to pass a national exit exam developed and administered by the Faculty of Physician Associates which includes a written assessment (a Single Best Answer, multiple choice paper) and a practical component (an OSCE examination of consulting, examination and procedural skills). Physician Associates do not undergo revalidation in the same way that GPs do, but instead have to pass the written component of this exit exam every six years to remain on the voluntary register. They are also required to have yearly appraisals by their employer. In addition, Physician Associates are required to complete 50 hours of CPD per year to remain on the voluntary register and it is recommended that they have an annual appraisal with a GP.
- UKIUBPAE provides a network for Higher Education Institutions which supports and enables them to meet, share best practice and review the training, assessment and standards for Physician Associate education in the UK.
Funding for Physician Associate education
- Across the UK, most students on Physician Associate courses largely self-fund their tuition costs. However, government funding across England has been inequitable with some programmes and students receiving tuition, bursaries and placement funds and others receiving placement funding only; some programmes receiving no funding. This is being currently being addressed by HEE and further details are anticipated in the near future.
- HEE’s funding for Physician Associate programmes in England is separate to its budget for GP training; HEE has reassured RCGP that it will have no impact on the latter, nor other practice staff training funds. However, if Physician Associates gain more of their training experience in general practice, training capacity will need to be increased to ensure GP training, and training of other established practice roles, is not impacted. This will require additional investment.
Pay and indemnity
- A newly qualified Physician Associate has been evaluated under Agenda for Change at Band 7 (around £31,000-£41,000). Higher level Physician Associates (usually requiring a minimum of five years experience) have been banded at 8a (around £40,000-£48,000). The vast majority of Physician Associates currently working in the UK are on Band 7, with only a few very experienced ones on Band 8.
- Physician Associates usually obtain their own indemnity from the medical defense organisations. For a salaried Physician Associate this may be paid for by the practice or by the Physician Associate.
- Many challenging regulatory and wider policy issues must be addressed for Physician Associates in general practice to work most effectively (Jackson, Schofield and Marshall 2016). The RCGP will work with governments across the UK, the Faculty of Physician Associates and our members to address these issues.
Regulation and revalidation of Physician Associates
- Physician Associates currently have no statutory regulation as a profession. However, in October 2017, the Department of Health published a consultation on whether Physician Associates should be regulated. RCGP has previously called for regulation for this profession and welcomes the consultation.
- Currently, a voluntary register of Physician Associates is held by the Faculty of Physician Associates. The faculty and all relevant experts strongly advise that GPs should require the Physician Associates they employ with be on the register. This assures them that the individual is either a UK or USA-trained Physician Associate, has passed the national examination, maintained their CPD, passed the re-certification exam if appropriate (required every six years) and has not, at least to the knowledge of the faculty, had any significant professional behaviour issues raised.
- The Faculty of Physician Associates estimates that approximately 80% of Physician Associates are currently on the voluntary register.
- Regulation of Physician Associates is necessary to maintain high standards of professionalism and quality and to ensure that GPs and patients can have confidence in Physician Associates. This would also provide a framework within which extending Physician Associate competencies could be considered and the benefits and risks evaluated, for instance, to encompass prescribing rights.
- Support for the professional regulation of Physician Associates has been indicated by numerous Royal Colleges (including RCGP and RCP), Health Education England (HEE), the General Medical Council (GMC), the Health and Care Professions Council (HCPC) and other stakeholders.
- As part of a new regulatory framework for Physician Associates, a framework for revalidation should be introduced. At present, Physician Associates retake the written component of their exit exam every six years. While this approach ensures they maintain a current level of medical knowledge, adopting a revalidation model once professional regulation has been established would help to ensure they are continuing to work safely and effectively.
Funding and support for the rollout of Physician Associates in general practice
- The profession is already growing rapidly; for example, over the past four years the number of Physician Associate courses has grown from 2 to 28. However, even with this growth, the target for England of 1,000 Physician Associates working in general practice by 2020/21 is unlikely to be achieved without significant intervention that goes beyond supporting the training of Physician Associates and supports their transition to employment as well.
- Governments could support the rollout of Physician Associates in general practice through a programme to provide funding and support to practices looking to employ a Physician Associate. This would allow for a consistent and supported approach. The government could evaluate support for the integration of the role into general practice over time.
- There may also be a role for the RCGP, in partnership with the Faculty of Physician Associates, to develop practical guidance for GPs looking to employ a Physician Associate. The Faculty of Physician Associates has recently published An Employers Guide to Physician Associates (PA) (Faculty of Physician Associates, 2017a). The guide is for both primary and secondary care, including some specific guidance for general practice as well as outlining the current limitations of the role and supervision requirements. This could be built upon to provide additional specific information for general practice, such as exemplar job descriptions. The RCGP has partnered with colleagues to develop similar resources for pharmacists, physiotherapists, and paramedics.
What supervision means in general practice
- One of the obvious challenges for effectively integrating Physician Associates into the general practice workforce is to fully understand what supervision arrangements might look like in a general practice context where Physician Associates have their own consultations with patients. The recently published Faculty of Physician Associates employer guidance may be useful for this, but further support could be developed. The relationship is likely to be similar to supervision of other advanced clinical practitioners who are seeing face-to-face patients.
- A further challenge is ensuring affordable and sufficient indemnity cover if available for supervisors of Physician Associates and practices employing these staff.
Ensuring equality of access to GPs
- Some concerns have been voiced that if Physician Associates are mainly employed in areas with severe shortages of GPs, they may end up clustered in deprived and/or rural areas. While patients in these areas would benefit from enhanced access to services within the practice, over time this could contribute to a variation in access to GPs across different parts of the UK. It will be important to monitor any geographical inequalities that might develop in any evaluation of the impact of Physician Associates in general practice. Physician Associates should not be considered a replacement for GPs within workforce planning in general practice.
- However, the role of Physician Associates may help to improve access for patients to general practice through helping to extend the availability of appointments to see a member of the practice team for ailments within the framework of Physician Associate competencies.
Considering patient preferences
- It is important that patient preferences are understood and acknowledged as Physician Associates are rolled out in general practice. A survey of the members of the RCGP’s Patient Groups across the UK found that, after the role of a Physician Associate was explained, patients were broadly comfortable with the idea of having a consultation with a Physician Associate in general practice. Many of the patients would choose to have an appointment with a Physician Associate quickly, rather than wait for an appointment with a GP. This is consistent with evidence that for same day appointments in general practice there were no significant differences in re-consultation rates nor diagnostic or prescribing activity between Physician Associate and GP appointments and the vast majority of patients were happy to see Physician Associates again for similar problems (Drennan, et al., 2015), (Farmer, Currie, West, Hyman, & Arnott, 2009), (Jackson, Schofield & Marshall, 2017).
- The responses of the members of the Patient Groups are summarised below:
| Strongly disagree | Disagree | Neither agree nor disagree | Agree | Strongly agree | |
| I would be comfortable having an appointment with a Physician Associate in general practice | 0% 0 |
0% 0 |
21.43% 3 |
57.14% 8 |
21.45% 3 |
| I would prefer to have an appointment with a Physician Associate quickly rather than wait a long time for an appointment with a GP | 0% 0 |
11.11% 2 |
16.67% 3 |
55.56% 10 |
16.67% 3 |
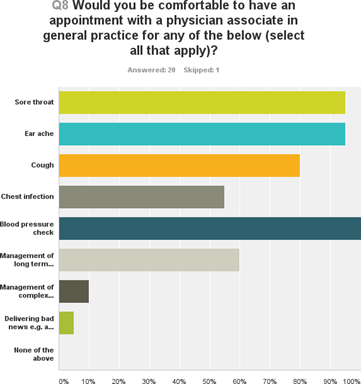
- While members of the Patient Groups were broadly comfortable with the idea of an appointment with a Physician Associate, this was not true for all medical issues. Patients tended to report that they would be comfortable having an appointment with a Physician Associate for issues including blood pressure checks, sore throat and management of a single long-term condition, but not for the management of complex multiple long-term conditions and or for receiving bad news such as a cancer diagnosis.
- Patient opinion may well further change over time as exposure to Physician Associates increases. Proactive measures to raise public awareness and understanding of the role will also be necessary in order to fully integrate Physician Associates into the general practice team on a wider scale.
Training Physician Associates for general practice settings
- Physician Associate courses vary greatly in terms of the time that Physician Associate students spend in general practice, although the national curriculum specifies a minimum of 180 hours, i.e. 5 weeks. There is strong evidence that spending time in general practice enhances students’ opinions of general practice and leads to more students choosing to work in general practice (Wass, 2016) (Alberti, 2017). The same is likely to be true for Physician Associates. In order to ensure that a significant proportion of Physician Associates choose to work in general practice after graduation, and that they have appropriate experience, more exposure to general practice is likely to be needed.
- Achieving more and longer placements in general practice will be a challenge. General practices may already be hosting medical students and student nurses (and exposure to general practice will be important for these professions). In order to achieve more placements in general practice, more funding will need to be made available to support practices in hosting Physician Associate students. There will also need to be significant investment in training general practice trainers.
The relationship between the RCGP and the Faculty of Physician Associates
- The Faculty of Physician Associates is hosted by the RCP, which received funding from HEE to host the new Faculty from 2015. There is scope for the RCGP to work more closely with the Faculty of Physician Associates in the future to support Physician Associates working in general practice, and the Faculty has stated that they are keen to develop a closer relationship with the RCGP.
Engaging with the regulatory and policy process
- RCGP will respond to the consultation on the regulation of Physician Associates during the consultation period, which ends on 22 December 2017. RCGP will continue to engage with governments across the UK. The Faculty of Physician Associates and the universities providing courses through the UK and UKIUBPAE as Physician Associates are rolled out in general practice and with HEE and its Medical Associate Professions Oversight Board.
Supporting our members
- The issues around the new role of Physician Associates indicate a broader challenge facing general practice: how to integrate a range of roles into the practice team effectively. There is a consensus that one of the solutions for freeing up GP time to focus on the most complex patients in primary care is to make use of allied healthcare professionals and other practice staff to handle more straightforward cases and much of the administrative burden. GPs will nevertheless require support to recruit, manage, supervise and use these expanded practice teams best.
- The College is well placed to help provide support and expertise in this area, working with the relevant professional bodies such as the Faculty of Physician Associates. For instance, an online toolkit could be developed to provide practical support to members, such as guides to employing different practice team members and job descriptions explaining the capabilities and limitations of various roles. It could also provide resources for continuing professional development.
- Supporting our members as leaders of the wider practice team is an ongoing area of work. This aligns with the Policy and Campaigns priorities for 2017/18 on workload and the interface between primary and secondary care, encompassing work around developing new care models.
Conclusion
The RCGP is committed to working with governments across the UK, the Faculty of Physician Associates and our membership to ensure that Physician Associates in general practice are safely and effectively integrated into the multidisciplinary team. Physician Associates provide a complementary rather than a substitute role to GPs. Their integration into general practice does not mitigate the need to address the shortage of GPs urgently, nor does it reduce the need for other practice staff. Instead, Physician Associates can help broaden the GP role's capacity and skill mix within the practice team to enhance patient care.
RCGP calls for the following steps to be taken forward to ensure the effective and safe integration of Physician Associates into general practice:
- Commitments in the GP Forward View relating to Physician Associates need to be met. These sit alongside commitments to increase the number of GPs
- Professional regulation needs to be established as a matter of urgency
- Once regulated, consideration needs to be given to enabling Physician Associates to acquire appropriate prescribing rights
- The level of exposure to general practice during Physician Associate courses needs to be evaluated and potentially extended
- Resources for training placements in general practice must be increased; accordingly, the training of GPs and other staff must not be affected
- Clearer guidance and support needs to be produced on effective supervision of Physician Associates, e.g., in out of hours settings
- Funding should be provided to practices to support Physician Associate’s transition into employment, e.g., for preceptorships
- Further research is needed on the cost, impact, and geographical distribution of Physician Associates
- Measures should be taken to raise public awareness and understanding of the Physician Associate role in general practice
Appendix 1: List of physician associate courses by nation
| England | |
| Anglia Ruskin University | Physician Associate MSc |
| University of Birmingham | Physician Associate Studies Diploma; Physician Associate Studies MSc |
| University of Bradford | Physician Associate Studies PG Diploma; Physicians Associate Studies MSc |
| Brighton and Sussex Medical School | Physician Associate Studies Postgraduate Clinical Diploma |
| Brunel University | Physician Associate MSc |
| Buckinghamshire New University | Physician Associate PGDip |
| Canterbury Christ Church University | Physician Associate Studies PgDip |
| University of Central Lancashire | Physician Associate Studies PgDip |
| University of Chester | Physician Associate MSc |
| University of East Anglia | Physician Associate Studies MSc |
| Hull York Medical School | Physician Associate Studies MSc |
| University of Leeds | Physician Associate Studies PgDip |
| University of Liverpool | Physician Associate Studies Postgraduate Diploma |
| University of Manchester | PGDip Physician Associate Studies |
| Newcastle University | Physician Associate Studies PGDip |
| Plymouth University Peninsula School of Medicine | PGDip Physician Associate Studies |
| Queen Mary University of London | Physician Associate Studies MSc |
| University of Reading | PGDip Physician Associate |
| Sheffield Hallam University | PgDip Physician Associate Studies |
| University of Sheffield | Postgraduate Diploma in Physician Associate Studies |
| St George's, University of London | Physician Associate Studies MSc |
| University of Surrey | Physician Associate PGDip |
| University of the West of England (UWE Bristol) | Physician Associate Studies MSc |
| University of the West of England (UWE Bristol) | Postgraduate Diploma in Physician Associate Studies |
| University of Wolverhampton | Postgraduate Diploma in Physician Associate Studies |
| University of Worcester | Physician Associate MSc |
| De Montfort University Leicester | Physician Associate Studies MSc |
| Northern Ireland | |
| Ulster University | Physician Associate Studies - PgDip/MSc |
| Scotland | |
| University of Aberdeen | Physician Associate Studies MSc |
| Wales | |
| Bangor University | Physician Associate MSc |
| Swansea University | PG Dip Physician Associate Studies |
List of institutions sourced from the Faculty of Physician Associates (now closed), accessed 8 August 2017
Bibliography
Alberti, H., Randles, H, Harding, A., McKinley, R. (2017). Exposure of undergraduates to authentic GP teaching and subsequent entry to GP training: a quantitative study of UK medical schools. British Journal of General Practice, e248-e252
British Medical Association. (2017). Physician Associates in the UK. London: British Medical Association.
Chartered Society of Physiotherapy, Royal College of General Practitioners, British Medical Association. (2016). General Practice Physiotherapy posts - a guide for implementation and evaluation. London: Chartered Society of Physiotherapy, Royal College of General Practitioners, British Medical Association.
Department of Health (2006) The Competence and Curriculum Framework for the Physician Assistant. London: Department of Health
Department of Health (2012). The Revised Competence and Curriculum Framework for the Physician Assistant. [Accessed 3 October 2017]
Department of Health. (2016). The Government Response to the House of Commons Health Select Committee Report on Primary Care (Fourth Report of Session 2015-16). London: Department of Health.
Drennan, V. M., Halter, M., Joly, L., Gage, H., Grant, R. L., Gabe, J., et al. (2015). Physician associates and GPs in primary care: a comparison. British Journal of General Practice, e234-e250.
Faculty of Physician Associates. [Accessed 10 August 2017]
Faculty of Physician Associates (2017a). An Employers Guide to Physician Associates (PA) [Accessed 10 August 2017]
Faculty of Physician Associates. (2017b). Physician Associate Managed Voluntary Register (PAMVR) [Accessed 4 August 2017]
Farmer, J., Currie, M., West, C., Hyman, J., & Arnott, N. (2009). Evaluation of Physician Assistants to NHS Scotland: Final Report. Inverness: UHI Millennium Institute.
General Medical Council. (2013). Good Medical Practice. General Medical Council.
Jackson, B., Schofield, S., Marshall, M. (2017). What are the Barriers and Facilitators to the integration of Physician Associates into the General Practice Workforce? – A grounded theory approach. British Journal of General Practice – in press.
NHS Digital. (2017), ‘Table 8b: General practice staff by type, full time equivalent, 2006-2016’, General and Personal Medical Services in England, Bulletin Tables 2006-2016. [Accessed 29 August 2017]
Parle, J. (2016) Personal communication, Chair of UK and Ireland Board for PA
Education Primary Care Pharmacy Organisation. (2016). A guide for GPs considering employing a pharmacist. London: Primary Care Pharmacy Organisation endorsed by the Royal Pharmaceutical Society and the Royal College of GPs.
Ritsema, T. (2014). Results of the Fourth Annual UK Physician Associate Census, London: Faculty of Physician Associates.
Ritsema, T. S. (2016). Faculty of Physician Associates Census results 2016. London: Faculty of Physician Associates, Royal College of Physicians
Wass, V. (2016). By Choice not by Chance. London: Health Education England.
Wilkie, P. V. (2016). Written evidence submitted to the House of Commons Health Committee inquiry into Primary Care. London: House of Commons.
Acknowledgements
This paper was developed with the help of a virtual expert working group of Physician Associates and GPs whose input was invaluable in informing the paper. Thank you to for your openness and generosity. Thank you also to members of the RCGP’s Patient Groups for your input.
- Prof. Kamila Hawthorne
- Dr Sue Rendel
- Prof. Jim Parle
- Dr Ben Jackson
- Christopher Deane
- Emma Lomas
Thank you for your feedback. Your response will help improve this page.