What are the CEPS requirements?
By the end of ST3, and to be awarded your CCT, evidence of the following must be included:
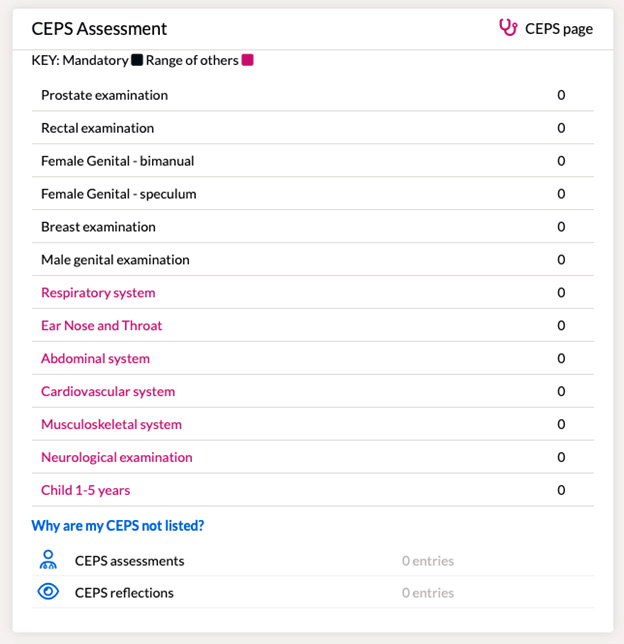
- The five mandatory intimate examinations (breast, rectal, prostate, female genital, (which includes a bimanual and speculum examination) and male genital examinations). A suitably trained professional will need to observe and document your performance on a CEPS evidence form.
- A range of additional Clinical Examinations and Procedural Skills relevant to General Practice which demonstrate clinical competence. 7 “system” GP focussed observed CEPS categories are included in the Clinical Examination and Procedural Skills section of the Portfolio (Respiratory system, Ear Nose and Throat, Abdominal system, Cardiovascular system, Musculoskeletal system, Neurological examination, Child 1- 5 years). For complete clarity, a range cannot be demonstrated with just 2 CEPS, nor could it be demonstrated with CEPS of only one type (i.e. 3 "ENT" CEPS). A suitably trained professional will need to observe and document your performance on a CEPS evidence form.
With clinical examination now only being assessed in WPBA, it is essential that sufficient evidence is provided to the Trainer/Educational Supervisor to feel confident in grading a trainee as competent in the capability of CEPs, and it will always be up to the judgement of the Trainer/Educational Supervisor as to what evidence is required for CEPS. As such, there are no set numbers for how many 'non-intimate'/'other'/'system' CEPS should be completed. However, being graded as "able to complete unsupervised" in all of the 7 "system" GP focussed observed CEPS in addition to the mandatory CEPS would provide strong evidence of competency in the capability of CEPS, and strong evidence that a trainee has met the CEPS requirements for WPBA.
In addition to the requirements for the end of ST3, throughout your training, you should be completing some, relevant to post, CEPS in each training year (ST1 and ST2). For complete clarity, if you had not completed any CEPS relevant to post, this would not allow you to meet the requirements for ST1 or ST2.
Your supervisor must also be satisfied through observed evidence or documented evidence from others that you are competent in general and systemic examinations for the clinical curriculum areas. These may well have been completed in your previous training but can be easily covered in joint surgeries for example.
Which CEPS skills need to be assessed?
By the end of training your Educational Supervisor must have observed or have documented evidence from others that you are competent in general and systemic examinations in the clinical curriculum areas.
There are 5 intimate examinations which need to be specifically included, as these are mandated by the GMC. These include breast, rectal, prostate, male genital examination and female genital examination (which includes a speculum and bi-manual pelvic examination).
You need to be observed performing the intimate examinations by a suitably trained professional. The assessor records their observation on the CEPS evidence form. If this is another doctor, they must be at ST4 level or above, or an SAS equivalent. If the assessor is another healthcare professional, such as a specialist nurse, they must confirm their role and training so that your Educational Supervisor can be satisfied that they have been appropriately trained.
You may also decide to write a separate log entry on any of these specific skills.
It is also important to note that this is not an exhaustive list of intimate examinations and indeed any examination can be considered intimate by some patients (for example, an examination of the eye with an ophthalmoscope), but the examinations listed are those that, due to their particularly intrusive nature, need to be specifically observed, and commented on, during your training.
The 5 mandatory examinations should not be considered as a ‘minimum requirement’ on their own and they cannot by themselves demonstrate overall competence in CEPS. A range of observed assessed CEPS which are relevant to general practice are also required. 7 “system” observed CEPS categories are included in the CEPS section of the Portfolio to help meet this requirement.
These are:
- Respiratory system
- Ear Nose and Throat
- Abdominal system
- Cardiovascular system
- Musculoskeletal system
- Neurological examination
- Child 1- 5 years
The image below shows how this appears on the Trainee Portfolio:
This again is not an exhaustive list, nor is there a set minimum number as everyone has different needs. You are expected to document your performance in CEPS in your portfolio and/or discuss your learning needs during placement planning meetings with your supervisors. The range of examinations, procedures and the number of observations will depend on your particular requirements and the professional judgement of your clinical and educational supervisors.
For example, you may recognise that your learning needs to include more experience of joint examinations, the examination of the eye, or doing a new-born baby check. You may wish to discuss with your supervisor how these can be addressed. Your supervisor may also recognise areas that need to be addressed such as completing a mental health state examination within a GP-length consultation or examining a diabetic patient’s feet correctly.
You may already be aware of specific CEPS you want to address, but these can equally become apparent during your consultations with patients.
In addition, it is important to recognise the procedures you may need during emergency presentations in general practice. For example, can you explain to a patient who is having an asthma attack what you are going to do in setting up a nebuliser, and set it up effectively?
Clinical Examination and Procedural Skills (CEPS) FAQs
There is no agreed definition of what constitutes an intimate examination. The five examinations for which evidence of competence is required by the GMC are generally accepted examples of intimate examinations, but there are many others. For instance, the examination of the eye with an ophthalmoscope is considered by many be an intimate examination, especially as it requires the examination room to be darkened. Ultimately it is the individual patient who determines what is intimate or invasive for them and this will be determined by a number of possible factors including their prior experiences, demographic and other factors.
The standard is that of an independent fully qualified General Practitioner. As well as the technical aspects of examination and the ability to recognise abnormal physical signs, it includes the choice of examination best suited to the clinical context. For instance, a competent GP very rarely performs an extensive neurological examination but will perform a limited neurological examination, as determined by the history taken from the patient, and perform it within the length of the GP consultation.
Training in a skills' lab and the use of manikins can be a very helpful adjunct to training in the workplace. In general, and certainly in the case of the five intimate examinations as required by the GMC, this will not be sufficient evidence of competence without the demonstration that your skills can be applied in a clinical context.
Although being observed performing such an examination might be helpful it would be unlikely to provide sufficient evidence of clinical competence. For instance, the extent of the examination in such a situation is determined by the insurance company and not by the clinician and may not be performed within the length of a normal GP consultation.
No, if your Educational Supervisor is satisfied that the evidence you have provided for one of the five intimate examinations as required by the GMC is sufficient this does not need to be repeated. However, it is important that this evidence is recorded in such a way that you can remember where it is. The easiest ways to do this is to use the CEPS forms. At the final review before a Certificate of Completion of Training (CCT) is recommended your Educational Supervisor will need to answer a specific question in relation to these examinations.
All GP trainees, including those with a disability, are to meet the required competences to ensure patient safety. This includes having the insight to:
- recognise when a disability prevents completion of an examination
- understand the examination required, and that it is a necessary part of the consultation
- facilitate a patient examination in a timely fashion
- demonstrate that the trainee knows what to do with the findings.
- If a trainee feels this guidance may apply to one of their examinations (regardless of whether it is a mandatory examination or not) they should discuss this with their Educational Supervisor/Programme Director in the first instance.
For example, one possible approach might be that a trainee who cannot physically carry out an examination refers the patient to a colleague, and then instruct the colleague to examine the patient appropriately, and then interpret the findings having communicated with the colleague who carried out the examination.
In a training context, to satisfy the CEPS requirement, the observer (who could be the person who performs the examination) should document on the assessment form the part of the CEPS they did observe, and document why it was necessary for the examination to be done in this way.
This should be added into the observation and feedback performance box on the assessment form.
No, evidence of a range of assessed CEPS is also required for your ES to sign off the capability of CEPS before CCT.